Thyroid: What HTMA tells us about your thyroid health
During the middle of my senior season as a division 1 college athlete, I had been severely struggling with my physical health - which had been happening on and off for the last 7 years. This time, I could barely digest my food, I wasn’t hungry, my metabolism felt stunted, I woke up exhausted every morning despite going to bed at 9 pm and waking up at 7 am, I couldn’t concentrate, and my had no control of my legs at practice. It was almost as if I couldn’t pick them up to run or move them the way I needed to as an athlete.
After weeks of feeling this way, I broke down crying in the middle of a drill. I couldn’t keep up any longer.
The team doctor asked me to get my bloodwork done. One marker she checked was my TSH levels to assess my thyroid health. I was also convinced this would show up abnormal in some way since I showed every symptom of thyroid dysfunction.
BUT EVERYTHING CAME BACK NORMAL!
Yes, that’s right. Not only did TSH come back normal, but the whole panel was fairly in range.
I was so confused. How could my bloodwork say that everything was normal? I felt so rundown. So tired. So heavy. And yet, I had nothing to show for it.
If nothing showed out of range, then why did I feel this way? I was eating unnecessarily healthy and clean. I was very strict with my diet, I was clearly exercising, and I was a non-toxic skincare product, personal care product, household cleaning supply, filtered water freak. I was doing more for my health than anybody I knew. So why was the needle never moving for me to feel better?
It wasn’t until I became a Functional Diagnostic Nutrition Practitioner that I realized how little I knew about my thyroid. We are taught to treat everything and every system in our body in isolation. This is a dangerous school of thought. The thyroid is in fact the weakest gland in the body. When other systems in our body become rundown, overburdened, or stressed, the thyroid takes the brunt of it.
So let’s dig a little deeper into how I found out I had cellular hypothyroidism and what I did to have a fully functional thyroid today.
Typically, a thyroid blood test is incomplete. Serum tests only measure 3 out of 7 markers. None of which are the most important. If you are looking to diagnose a thyroid issue, you would need to get a FULL thyroid panel, which many doctors do not order!
Doing a full thyroid panel can be helpful if you are looking for additional information, but it doesn’t tell you WHY this is happening.
When it comes to thyroid dysfunction, whether that is an overactive (hyperthyroid) or an underactive (hypothyroid) state, you should ALWAYS looking at mineral levels when it comes to supporting and balancing it.
For example:
If your HTMA test shows high tissue calcium, then calcium is blocking the thyroid hormone in its active form from getting into the cells and actually doing its job to make energy for the for the body.
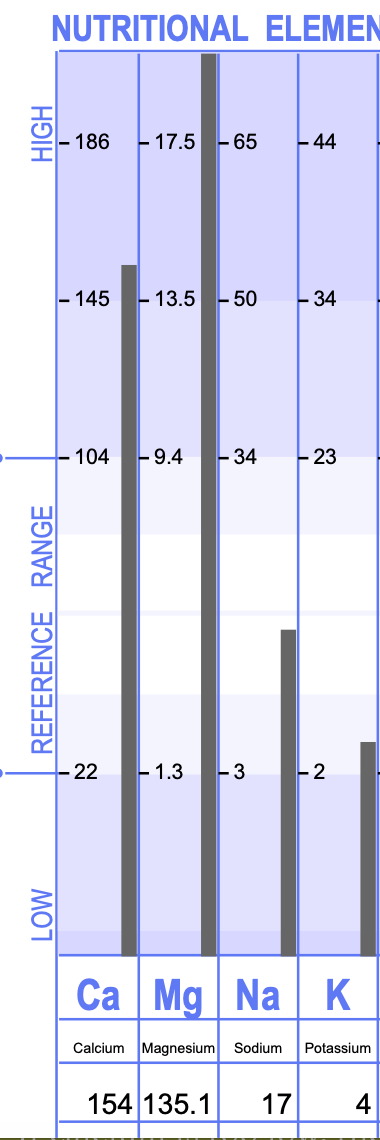
This is shown below.
Make it stand out
Whatever it is, the way you tell your story online can make all the difference.
The client above had cellular hypothyroidism. No autoimmunity as in the case of Hashimoto’s, and not a hypothyroid diagnosis. This is a perfect example of why her levels on a blood test would show normal, but in reality, there is underlying thyroid dysfunction at the cellular level. Calcium is so high, it causes a calcium shell. This blocks T4 to T3 conversion. When a calcium shell is present, or if calcium is higher than we would like to see, this often means that calcium has built up in the tissues of the body, rather than the bones and teeth where it should be causing numerous health issues.
Additionally, potassium is so low, it doesn’t allow the cell to be sensitized. The thyroid hormone that IS converted and activated cannot enter the cell properly because of this low potassium level.
On the other hand, if calcium is too low, then thyroid hormone conversion is happening too often and getting into the cell too frequently leading to an overactive thyroid.
We can’t just look at calcium or potassium either. There are several other micronutrients that play a large role in thyroid hormone conversion, cell sensitization, and retention of these necessary minerals.
For example, if selenium is depleted, then there is no T4 to T3 conversion.
If iodine is low, then there is no T4 to T3 conversion. Low iodine levels can also cause a calcium shell build-up.
Here’s the catch - Don’t just start taking all of the supplements and minerals you can get. I have seen this before. For example, clients take dessicated beef liver, causing there copper levels to skyrocket when there was already hidden copper toxicity in the body. Or clients take Cal/Mag supplements when they already have high calcium in the tissue that needs to be removed, and put back into the bones. It is important to get an assessment of your mineral status, and get the support that YOUR body needs.
You cannot heal the thyroid long-term without addressing mineral balance. You can put a band-aid on the issue with thyroid medications, or you can address the root cause. If left unaddressed, the thyroid is the weakest gland in the body, and eventually can destroy its own tissue.
This is why I would recommend doing an HTMA test. It measures over 37 viral minerals, showing the state of your thyroid status and the WHY behind your symptoms.